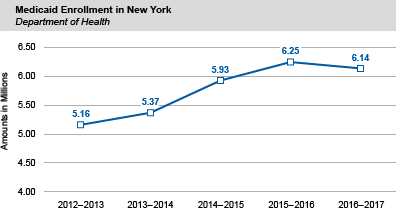
Medicaid Enrollment Decreases for the First Time in Nine Years
- Average monthly enrollment in the State’s Medicaid program exceeded 6.1 million in SFY 2016-17, a decrease of 112,741, or 1.8 percent, compared to the prior year. The decrease, the first since 2008, was due in part to the transfer of certain lawfully present immigrants previously covered by Medicaid to the Essential Plan (see below).
- Compared to the prior year, average monthly enrollment for:
- Adults decreased by 166,306 (6.3 percent) to 2.5 million, accounting for the largest decrease in enrollment;
- Children with Medicaid coverage decreased by 4,433 (0.2 percent) to 2.2 million;
- Elderly recipients increased by 81,902 (15.8 percent) to 599,923;
- Blind or disabled recipients decreased by 57,796 (7.7 percent) to 692,749; and
- “Other” eligible recipients, largely legal immigrants, increased by 33,893 (25.9 percent) to 164,574.
- Medicaid recipients enrolled in managed care plans at the end of March 2017 increased by 15,119 (0.3 percent) to nearly 4.7 million, or 76.4 percent of all recipients, compared to March 2016. This increase reflects the continued enrollment of most new recipients into managed care plans and the continued transition of certain populations from fee-for-service to Medicaid managed care. As of the end of March 31, 2017, 76.4 percent of all Medicaid recipients were enrolled in managed care plans.
Medicaid Spending Increases, Largely Due to Additional Federal Payments from the Federal Affordable Care Act (ACA)
- Compared to last year, combined local, State and federal spending on Medicaid claims increased by $2.4 billion (4.3 percent) to $60.1 billion. This increase largely reflects additional federal Medicaid payments, most of which are associated with the ACA.
- Children and adults represented 76.2 percent of all average monthly enrollees, but only 41.7 percent of the overall costs of Medicaid claims for the State. Elderly, blind and disabled enrollees made up 21.1 percent of eligible recipients, but accounted for 55.9 percent of Medicaid claims costs.
The Essential Plan Continues to Grow
- In SFY 2016-17, enrollment in the Essential Plan averaged 674,478, an increase of 207,864 (44.5 percent) over the prior year.
- In 2015, New York State joined Minnesota to become the only states in the nation to establish a Basic Health Program, a new low-cost health insurance option authorized by the ACA and largely funded by the federal government. In New York State, the Basic Health Program is known as the Essential Plan.
- The Essential Plan is available to individuals who are under 65, not eligible for Medicaid or the Child Health Plus Program, without access to affordable coverage and with incomes at or below 200 percent of poverty.
- In SFY 2016-17, federal funds covered 91.2 percent of nearly $3.6 billion in Essential Plan costs, with State funds covering the remaining 8.8 percent. Individuals with incomes greater than 150 percent but at or below 200 percent of poverty pay $20 monthly premiums to private health plans participating in the program. Individuals with incomes at or below 150 percent of poverty have no monthly premium.
- All participating health plans cover inpatient and outpatient care, physician services, diagnostic services and prescription drugs with low out-of-pocket costs and no annual deductible. Enrollees have no out-of-pocket costs for preventive care, including routine office visits and recommended screenings.
*Numbers may not add due to rounding.